The majority of symptomatic disc herniations are found at the lower two lumbar interspaces, that is, about 50% at L4–5 and 47% at L5-S1 (1). The remaining 3% are found at higher lumbar levels (1). A research study comparing patients with upper lumbar (L1–2 and L2–3) herniations to those with herniations at L3–4, L4–5, and L5-S1, showed that the patients with upper lumbar herniations had frequently undergone disc surgery and that the surgical outcomes were significantly poorer (2). This could possibly be due to a relatively greater prevalence of asymptomatic disc herniations in the upper lumbar region.
These results provoke two questions:
1. Why are disc herniations diagnosed so rarely in the upper lumbar region?
2. Why are lower lumbar disc herniations diagnosed more frequently in the lower lumbar region?
So, two possible anatomical explanations can be given, both involving the relative vulnerability of the nerve root to compression by upper and lower lumbar herniations respectively. Here are my thoughts about this:
There are two possible anatomical explanations that can be given about “Why are disc herniations diagnosed so rarely in the upper lumbar region?”
First, in the upper lumbar region, the root sleeve is located well below the disc level. An upper lumbar herniation impinging upon the dural sac will tend to displace rather than compress the upper lumber root, as the roots have more freedom of movement in the transverse plane (3).
Also, in the upper lumbar region, the oval shape of the canal and the dural sac without lateral recesses may be the reasons for lower rates of nerve root compression (3).
But, this does not necessarily mean that disc herniations in the upper lumbar regions occur so rarely, but it could be that they cause symptoms less frequently.
What about lower lumber nerve roots? “Why are disc herniations diagnosed more frequently in the lower lumbar region?”
The reason for the frequent diagnosis of disc herniations in the lower lumbar region could be related to the point of emergence or axilla of the root sleeve relative to the disc.
In the lower lumbar region, the axilla of the root sleeve is located much closer to the disc level. This is more common at the L5/S1 level, frequently even above this level. Therefore, a lower lumbar herniation is much more likely to compress the nerve root (3).
Another factor is the presence of a lateral recess:
At L4/5 & L5/S1, where most disc herniations occur, the shape of the spinal canal is “triangular”. Therefore, there is a clearly defined lateral recess in the lower lumbar region (3). These lateral recesses tend to fix the root sleeve in place and prevent the nerve root from moving backward out of harm’s way when encroachment by a herniated disc takes place (3).
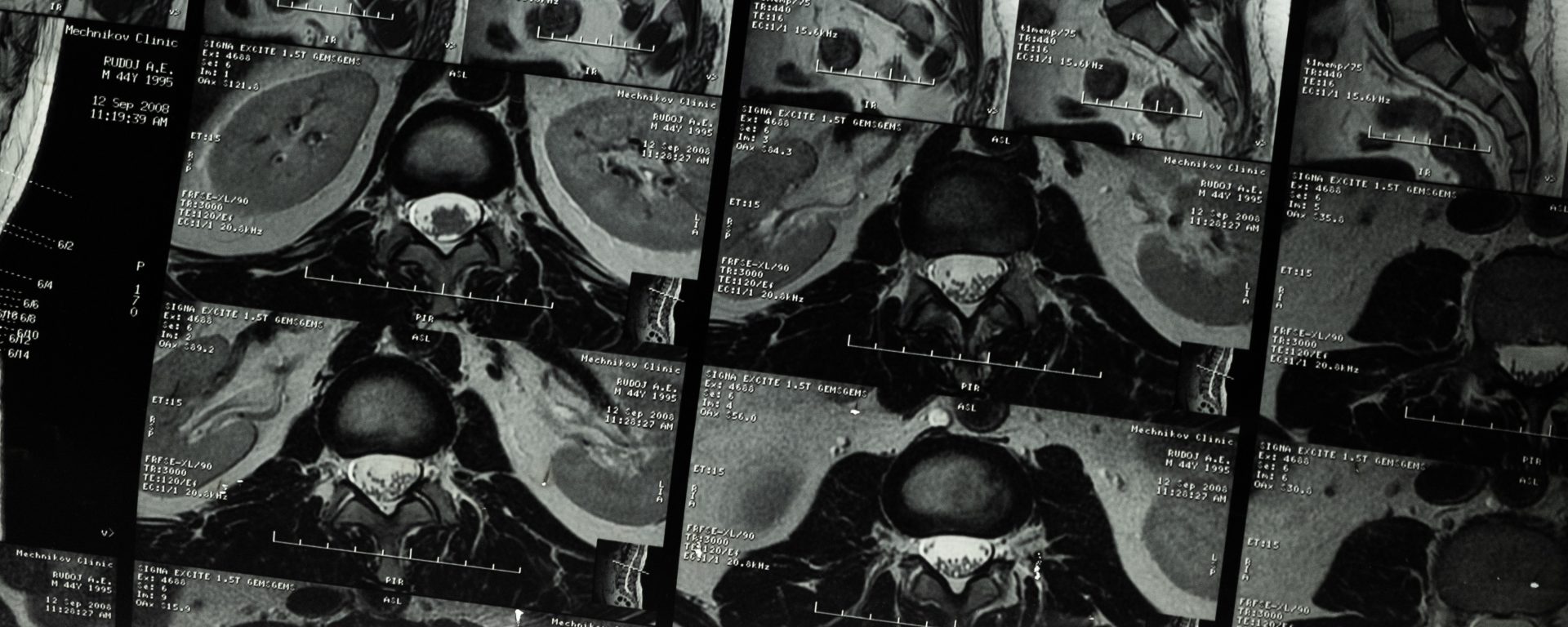
Next, in a group of asymptomatic volunteers (n=32) with disc degeneration or protrusion (41%) at the L3 to S1 levels, the lumbar dural sac volume increased with the increasing pressure of the cerebrospinal fluid and the increasing dural sac cross-sectional area as the posture changed from supine lying to standing position (4). At L3/4, L4/5, and L5/S1 levels, the mean dural sac cross-sectional area was significantly smaller in the supine position than in other upright postures (4). Notably, the increase in the dural sac cross-sectional area at the L5/S1 level was the most (or maximal) as the posture changed from supine to standing upright (4). In other words, the dural sac cross-sectional area decreased the most at the L5/S1 level due to the positional change from standing upright to a supine position (4). Therefore, a significant posture-dependent difference in the dural sac cross-sectional area at the level of L3 to S1 levels in combination with the factors mentioned above may be another reason for higher rates of ‘symptomatic’ disc protrusion at the lower lumbar levels (3, 4).
References:
1. Spangfort EV (1972) The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand Suppl 142:1.
2. Sanderson SP, Houten J, Errico T et al (2004) The unique characteristics of “upper” lumbar disc herniations. Neurosurgery 55(2):385.
3. McKenzie R, May S. The lumbar spine: mechanical diagnosis and therapy. 2nd ed. Waikanae: Spinal Publication Ltd; 2003.
4. Hirasawa Y, Bashir WA, Smith FW, Magnusson ML, Pope MH, Takahashi K. Postural changes of the dural sac in the lumbar spines of asymptomatic individuals using positional stand-up magnetic resonance imaging. Spine. 2007 Feb 15;32(4):E136-40.