Johann Friedrich Horner originally described the Horner syndrome (HS) in humans in 1869 (van der Wiel HL. 2002). HS is caused by a disruption in the oculosympathetic circuit between the hypothalamus and the orbit (Amonoo-Kuofi HS, 1999). The characteristic trio of ipsilateral eyelid ptosis, miosis, and face anhidrosis is what distinguishes HS. There are numerous causes of HS, but herniated cervical disc (HCD) is a fairly rare one.
The oculosympathetic circuit starts with a first-order neuron in the hypothalamus’s posterior lateral aspect and extends down the spinal cord from C8 to T2. A second-order (preganglionic) neuron exits the spinal cord via the ventral roots and enters the paravertebral sympathetic chain from the intermediolateral grey material of the spinal cord at level C8-T2 (Budge-Waller’s Cilionospinal Centre). The preganglionic pathway crosses the apex of the lung and ascends through the cervical sympathetic chain to the superior cervical ganglion. The superior cervical ganglion’s third-order (postganglionic) neuron, located at C2-C3, posterior to the carotid sheath and anterior to the longus colli muscle, travels through the carotid plexus into the skull, where it connects with the ophthalmic nerve and enters the orbit. HS may arise as a result of an injury anywhere along the route (Amonoo-Kuofi HS. 1999; Lee JH, et al. 2007; Reede DL, et al. 2008).
A HS can be classified as central (first-order neuron), preganglionic (second-order neuron), or postganglionic (third-order neuron) based on the location of the interrupted oculosympathetic pathway.
Central HS can be caused by brain stem ischemia, brain tumours, demyelinating disorders, syringomyelia, or transverse myelitis (Amonoo-Kuofi HS, 1999; Kerrison JB et al., 2000). Central HS is rarely seen in isolation. First-order neuron fibres pass in Budge’s centre, directly lateral to the dorsal grey matter, and synapse in the spinal cord grey matter (Reede DL et al. 2008).
Preganglionic HS can be caused by a thoracic or neck tumour, spinal cord trauma, herniated disc at C8-T1, iatrogenic sympathetic pathway disruption (e.g., radical neck dissection, selective nerve root block, carotid angiography, stenting, or endarterectomy), spontaneous carotid dissection, and aortic aneurysm, as well as malignant conditions that affect normal sympathetic innervations (Kaplowitz K, and Lee AG. 2011; Lee JH, et al. 2007; Miura J, et al. 2003; Montgomery DM, and Brower RS. 1992; Reede DL, et al. 2008; Russell JH, et al. 2009; Walton KA, and Buono LM. 2003; Zhao CQ, et al. 2007). Tumours or trauma are the most common causes of the preganglionic type.
Postganglionic HS can be caused by vascular headaches, a tumour or aneurysm in the cavernous sinus, a nasopharyngeal tumour, or trauma accompanying a basal skull fracture. The most common causes include carotid artery dissection and cluster headaches. However, most postganglionic lesions are idiopathic. Anhidrosis is rarely apparent, and in the postganglionic subtype, it is nearly absent (Amonoo-Kuofi HS. 1999; Reede DL, et al. 2008).
HCD is a prevalent cause of spinal cord compression; however, HS linked with HCD has only been recorded in a few studies. Only two cases of herniated thoracic disc at T1-2 were the aetiology of HS (Gelch MM. 1978; Lloyd TV, et al. 1980). Cervical herniated disc-related HS were extremely rare; I have found just two cases documented in the literature (Lee JH, et al., 2007; Russell JH, et al., 2009; Ma H, et al., 2012). Spinal cord compression is associated with cervical disc herniation at C4-C5 or C5-C6 levels, which causes an insult to the sympathetic system and may be a cause of HS (Lee JH, et al., 2007; Russell JH, et al., 2009; Ma H, et al., 2012). The HCD may directly compress the spinal cord, causing an injury to the sympathetic pathway’s first-order neuron at C4–C5. Patients with HCD frequently have neck pain, cervical radiculopathy, myelopathy, or a combination of these symptoms. However, if individuals have no cervical symptoms at all, this uncommon presentation might lead to a delayed or inaccurate diagnosis in a variety of directions. For example, because the patient had no cervical symptoms at first, the doctor suspected a brain stroke.
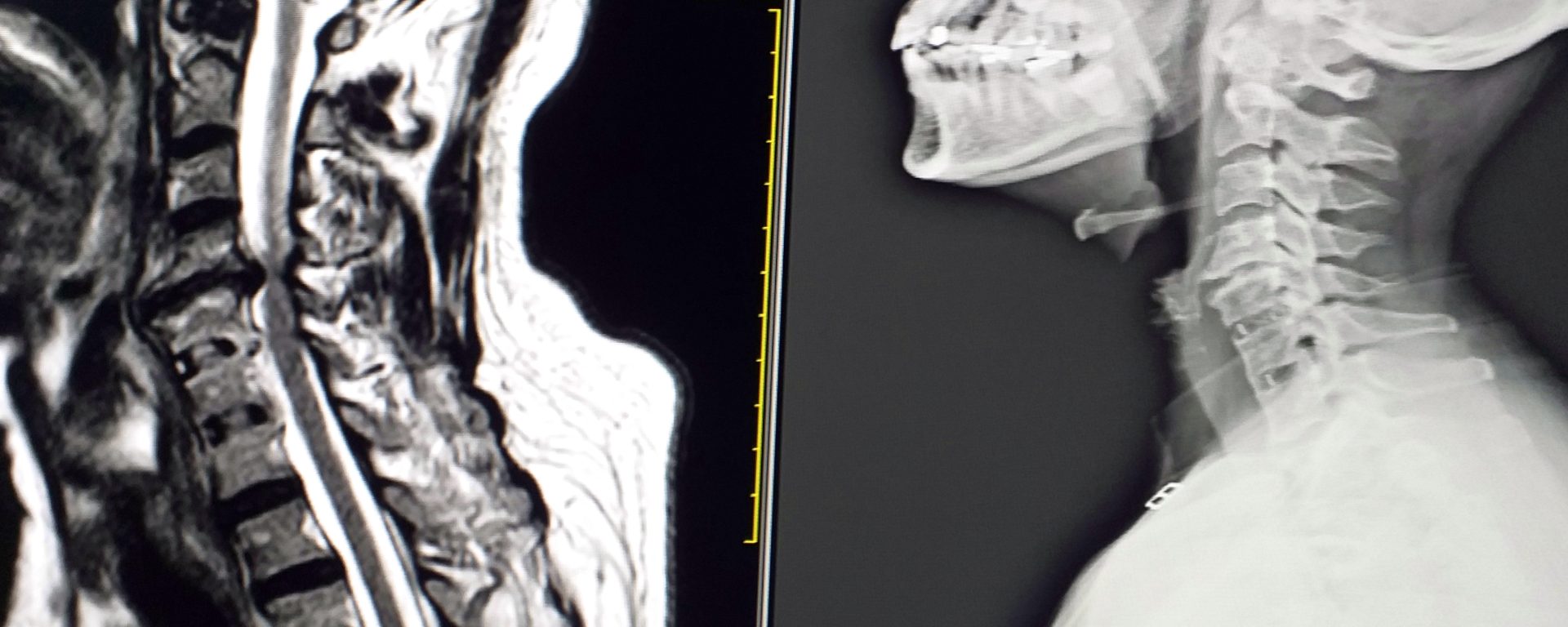
MR imaging is the most reliable investigative technique and should be used as the first diagnostic tool for HS associated with HCD. Early diagnosis and surgical decompression are required for therapy, since severe cord compression will result in additional neurological impairments.

References
- Amonoo-Kuofi HS: Horner syndrome revisited: with an update of the central pathway. Clin Anat 12:345-361, 1999.
- Gelch MM: Herniated thoracic disc at T1-2 level associated with Horner’s syndrome. J Neurosurg 48:128-130, 1978.
- Kaplowitz K, Lee AG: Horner syndrome following a selective cervical nerve root block. J Neuroophthalmol 31:54-55, 2011.
- Kerrison JB, Biousse V, Newman NJ: Isolated Horner’s syndrome and syringomyelia. J Neurol Neurosurg Psychiatry 69: 131-132, 2000.
- Lee JH, Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC: Neuroimaging strategies for three types of Horner syndrome with emphasis on anatomic location. AJR Am J Roentgenol 188: W74-81, 2007.
- Lloyd TV, Johnson JC, Paul DJ, Hunt W: Horner’s syndrome secondary to herniated disc at T1-T2. AJR Am J Roentgenol 134:184-185, 1980.
- Ma H, Kim I. Horner Syndrome associated with a Herniated Cervical Disc: a case report. Korean J Spine 2012; 9: 108–110.
- Miura J, Doita M, Miyata K, Yoshiya S, Kurosaka M, Yamamoto H: Horner’s syndrome caused by a thoracic dumbbellshaped schwannoma: sympathetic chain reconstruction after a one-stage removal of the tumor. Spine 28(2):33-36, 2003.
- Montgomery DM, Brower RS: Cervical spondylotic myelopathy. Clinical syndrome and natural history. Orthop Clin North Am 23:487-493, 1992.
- Reede DL, Garcon E, Smoker WR, Kardon R: Horner’s syndrome: clinical and radiographic evaluation. Neuroimaging Clin N Am 18:369-385, 2008.
- Russell JH, Joseph SJ, Snell BJ, Jithoo R: Brown-Sequard syndrome associated with Horner’s syndrome following a penetrating drill bit injury to the cervical spine. J Clin Neurosci 16:975-977, 2009.
- van der Wiel HL: Johann Friedrich Horner (1831-1886). J Neurol 249:636-637, 2002.
- Walton KA, Buono LM: Horner syndrome. Curr Opin Ophthalmol 14:357-363, 2003.
- Zhao CQ, Jiang SD, Jiang LS, Dai LY: Horner Syndrome due to a solitary osteochondroma of C7: a case report and review of the literature. Spine 32(16):471-474, 2007.