Neurodynamic techniques are widely used as part of a multimodal strategy for treating patients with compression neuropathies. In this blog, I will cover various neurodynamic treatment choices as well as some clinical rationale considerations for their use, as well as what pathophysiological processes may be altered by treatment.
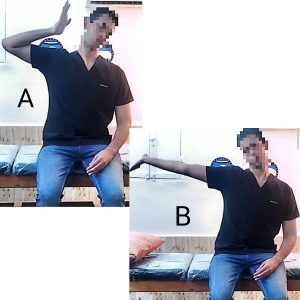
Neurodynamic procedures are approaches that try to mobilise either the nervous system itself or the tissues that surround it. Techniques for sliding and tensioning The neural system is mobilised by sliding and tensioning techniques (Butler DS. 2000; Coppieters MW, et al. 2008), whereas the structures around the nervous system are mobilised by a cervical contralateral lateral glide technique (Elvey R. 1986).
Sliding and Tensioning Techniques
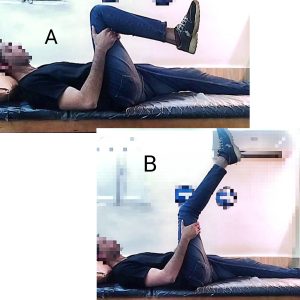
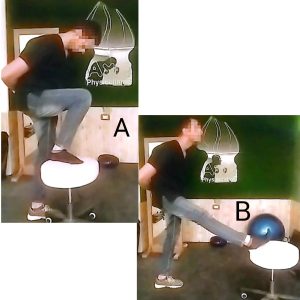
A sliding technique involves moving at least two joints at the same time, either actively or passively, in such a way that one movement counterbalances the increase in nerve strain generated by another (Butler DS. 2000). Sliding approaches are associated with substantially bigger nervous system excursions relative to surrounding structures but without potentially large increases in nerve strain (Butler DS. 2000).
Although the biomechanical effects of sliding and tensioning techniques on the nervous system are extremely different, it is crucial to note that one type of approach is not always preferable to the other (Coppieters MW et al. 2008). Sliding techniques are less intense and may be better suited for more irritable conditions; tensioning techniques may have a place in the later stages of recovery or in more sport-specific rehabilitation. Currently, there is very little comparative clinical evidence to inform procedure selection. Sound clinical reasoning, possibly erring on the side of caution, remains critical.
Mobilization of Surrounding Structures
Elvey first described the cervical contralateral lateral glide technique as a therapy strategy for neuropathic diseases (Elvey R. 1986). The technique’s immediate effects have been studied in a variety of conditions, including nerve-related neck and/or arm pain (Coppieters MW, et al. 2003) and musculoskeletal conditions such as lateral epicondylalgia (Vicenzino B, et al. 1996) and chronic whiplash-associated disorders (Sterling M, et al. 2010). When provided to individuals with peripheral nerve sensitization, the analogous approach for the lumbar spine—a segmental lumbar lateral flexion contralateral to the uncomfortable side—has likewise shown favourable results (Schäfer A. et al. 2011).
Indications
Elvey (Elvey RL. 1997) suggested a collection of signs and symptoms to support the idea of a ‘neurogenic condition’ that might be managed with physiotherapy. These were the criteria:
(a) an active movement impairment caused by noncompliance with a specific nerve;
(b) a passive movement disorder that is linked to the active malfunction;
(c) a positive neurodynamic test result;
(d) an aberrant nerve palpation response;
(e) indications of musculoskeletal dysfunction indicating that the source of the neurogenic condition is amenable to physiotherapy
(f) a protective stance that reduces the length of the afflicted nerve’s anatomical route.
Researchers have long been urged to find variables that predict whether a patient will respond to a treatment (Foster N. et al., 2009; Goldstein M. et al., 2011). Schäfer et al. (2011) and Nee et al. (2013) presented early data on features that may aid in the identification of patients with lumbar or cervical radicular pain who are likely to benefit from neurodynamic treatment. Patients with physical signs of increased nerve mechanosensitivity (e.g., reproduction of symptoms with neurodynamic testing and a change in these symptoms with structural differentiation, increased sensitivity to nerve palpation), no neurological signs, and no neuropathic pain qualities (i.e., Arabic version of clinician-administered or self-reported version of the Leeds Assessment of Neuropathic Symptoms and Signs score 12) are likely to improve with neuropathic pain treatment. Older age and lower impairments in median nerve neurodynamic test ROM in the involved limb relative to the uninvolved limb are similarly related to recovery in individuals with cervical radicular pain (Nee et al. 2013).
Influences on pathobiological processes
preliminary data on the putative operating mechanisms of neurodynamic methods.
- Impaired Nerve Movement Rehabilitation.
- Intraneural edoema evacuation.
- Extraneous oedema and pressure are reduced.
- Inflammatory mediators are dispersed.
- The Neuro-Immune Response is influenced.
- Descending Modulation Facilitation.
Clinical trial evidence
Patients with lumbar radicular discomfort benefit from adding SLR or slump ‘tensioning’ techniques to a lumbar mobilisation and exercise plan (Adel S. 2011; Cleland J. et al. 2006; Nagrale A. et al. 2012). According to one clinical investigation, neurodynamic therapy after lumbar surgery may not be beneficial (Scrimshaw S. et al. 2001). Patients with cervical radicular discomfort benefit more from neurodynamic treatment than from counselling to be active (Nee R. et al. 2012). Neurodynamic treatment effects are less positive for people with upper or lower limb peripheral neuropathic pain disorders. Although neurodynamic treatment appears to be superior to no treatment for CTS patients, it is not superior to other therapies (e.g., carpal bone mobilisation, splinting) (Page M. et al. 2012). Adding neurodynamic treatments to other interventions like splinting and tendon gliding exercises has little effect on outcomes (Page M. et al. 2012). These findings hold true whether neurodynamic techniques are used to move the entire upper limb or merely the wrist and hand. Patients with cubital tunnel syndrome may not benefit from neurodynamic therapy. In patients with mild to moderate symptoms, adding nerve gliding exercises to instruction on the pathomechanics of cubital tunnel syndrome and recommendations to avoid aggravating activities did not enhance 6-month results (Svernlov B. et al. 2009). However, Approximately 30% of participants were lost to follow-up and were not included in the statistical analysis, which could have influenced the results. In patients with mild to moderate symptoms, adding nerve gliding exercises to instruction on the pathomechanics of cubital tunnel syndrome and recommendations to avoid aggravating activities did not enhance 6-month results (Svernlov B. et al. 2009). However, over 30% of participants were not followed up with and were not included in the statistical analysis, which could have influenced the results.
Finally, neurodynamics (and other movement-based therapies) can help individuals with chronic neuropathic pain address both peripheral and central causes.

References
- Elvey RL. Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. J Hand Ther 1997;10(2):122–9.
- Butler DS. The Sensitive Nervous System. 1st ed. Unley, S. Aust.: Noigroup Publications; 2000.
- Coppieters MW, Butler DS. Do ‘sliders’ slide and ‘tensioners’ tension? An analysis of neurodynamic techniques and considerations regarding their application. Man Ther 2008;13(3):213–21.
- Elvey R. Treatment of arm pain associated with abnormal brachial plexus tension. Aust J Physiother 1986;32:225–30.
- Coppieters MW, Stappaerts KH, Wouters LL, et al. The immediate effects of a cervical lateral glide treatment technique in patients with neurogenic cervicobrachial pain. J Orthop Sports Phys Ther 2003;33(7):369–78.
- Coppieters MW, Stappaerts KH, Wouters LL, et al. Aberrant protective force generation during neural provocation testing and the effect of treatment in patients with neurogenic cervicobrachial pain. J Manipulative Physiol Ther 2003;26(2):99–106.
- Vicenzino B, Collins D, Wright A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain 1996;68(1): 69–74.
- Sterling M, Pedler A, Chan C, et al. Cervical lateral glide increases nociceptive flexion reflex threshold but not pressure or thermal pain thresholds in chronic whiplash associated disorders: a pilot randomised controlled trial. Man Ther 2010;15(2):149–53.
- Schäfer A, Hall T, Muller G, et al. Outcomes differ between subgroups of patients with low back and leg pain following neural manual therapy: a prospective cohort study. Eur Spine J 2011; 20:482–90.
- Adel S. Efficacy of neural mobilization in treatment of low back dysfunctions. J Am Sci 2011;7(4):566–73.
- Cleland J, Childs J, Palmer J, et al. Slump stretching in the management of non-radicular low back pain: a pilot clinical trial. Man Ther 2006;11(4):279–86.
- Nagrale A, Patil S, Gandhi R, et al. Effect of slump stretching versus lumbar mobilization with exercise in subjects with nonradicular low back pain: a randomized clinical trial. J Man Manipulative Ther 2012;20:35–42.
- Scrimshaw S, Maher C. Randomized controlled trial of neural mobilization after spinal surgery. Spine 2001;26(24):2647–52.
- Nee R, Vicenzino B, Jull G, et al. Neural tissue management provides immediate clinically relevant benefits without harmful effects for patients with nerve-related neck and arm pain: a randomised trial. J Physiother 2012;58:23–30.
- Page M, O’Connor D, Pitt V, et al. Exercise and mobilisation interventions for carpal tunnel syndrome (Review). Cochrane Database Syst Rev 2012;(6):Art. No.:CD009899.
- Svernlov B, Larrson M, Rehn K, et al. Conservative treatment of the cubital tunnel syndrome. J Hand Surg 2009;34E:201–7.
- Foster N, Dziedzic K, van der Windt D, et al. Research priorities for non-pharmacological therapies for common musculoskeletal problems: nationally and internationally agreed recommendations. BMC Musculoskelet Disord 2009;10:3.
- Goldstein M, Scalzitti D, Craik R, et al. The revised research agenda for physical therapy. Phys Ther 2011;91:165–74.
- Nee R, Vicenzino B, Jull G, et al. Baseline characteristics of patients with nerve-related neck and arm pain predict the likely response to neural tissue management. J Orthop Sports Phys Ther 2013;43(6):379–91.