Hip pain can have multiple causes, including non musculoskeletal, lumbosacral spine, intra-articular, and extra-articular. A consensus declaration has defined an evaluation algorithm for distinguishing the musculoskeletal causes of regional hip pain (Takla A et al. 2020). Lumbosacral and extra-articular diseases frequently coexist with intra-articular hip causes of pain (Takla A et al. 2020). As a result, a grasp of the complicated connections of the spine, pelvis, hip joint, and the entire lower quadrant is required. Delays in accurately identifying the origin of hip pain might prolong suffering and worsen the disease (White, S. G. 2016). Physiotherapists, doctors, and orthopaedic surgeons continue to struggle with accurately diagnosing the source of hip pain (Clohisy et al., 2009; McCarthy & Busconi, 1995; Reiman et al., 2013; Reiman et al., 2014b; Tijssen et al., 2012). According to Byrd and Jones (2001), up to 60% of patients with hip joint pain are initially misdiagnosed. Furthermore, some hip pathology has been linked to the development of other, more significant hip diseases (for example, labral tears leading to articular delamination and degenerative joint disease, and femoroacetabular impingement leading to osteoarthritis). This suggests that a more accurate and timely diagnosis could help delay or stop this progression (Ganz et al., 2008; McCarthy et al., 2001).

Due to a lack of relevant, high-quality diagnostic accuracy studies, no conclusive recommendations can be made regarding the value of information gathered from clinical hip examinations (Burgess et al., 2011; Rahman et al., 2013; Reiman et al., 2014a; Reiman et al., 2013; Tijssen et al., 2012). Thus, there is a need for high-quality research into the diagnostic utility of the clinical examination of the hip so that health professionals involved in the diagnosis and treatment of people suffering from hip joint pain can be confident that their decisions are based on accurate and valid test results. Clinical examinations could identify hip pain without expensive and invasive diagnostic procedures (Jaeschke et al., 1994a; Leeflang et al., 2008; Martin et al., 2010b; McCarthy & Busconi, 1995; Tibor & Sekiya, 2008).
In this section, I will summarize clinical findings from a doctorate thesis by S. G. White (2016) on the diagnostic accuracy of clinical examinations of the hip:
- The author of this thesis employed a positive anaesthetic response (>80% decrease in pain intensity reported during physical testing) as the reference standard for diagnostic accuracy.
- The key goals of this thesis were to determine the diagnostic accuracy of information collected from the history and physical examination of the hip, as well as that gained from a magnetic resonance arthrogram:
This research shows that most physical examinations are sensitive, not specific. The quadrant test has the most diagnostic utility, as it accurately screens for intra-articular disease with negative results. This study also revealed the value of information gained from the patient’s history, with the absence of dominating pain in the groyne ruling out symptomatic intra-articular disease and the presence of crepitus detecting this pathology. The clinical prediction rule produced from the clinical examination data represented the patient’s history’s worth. Four variables discovered came from history i.e. crepitus, dominant pain in the groin, age >39 and self-reported limitation of ROM. Only physical findings were included: a positive quadrant test and an internal rotation ROM less than 41°. In this study, the probability of a positive assessment for post-anaesthetic response rose to over 80% when the screening score reached 4 or higher. For patients with this score, we suggest considering referral for a guided intra-articular anaesthetic injection if contemplating surgery. Conversely, a score of 3 or lower appears insufficient to warrant early referral for diagnostic injections, MR imaging, or surgical consultation. These guidelines aim to optimize resource allocation, minimizing unnecessary investigations and treatments while expediting the identification of intra-articular pathology necessitating prompt specialist intervention. The model exhibited an overall accuracy of 81%, with a sensitivity of 91% and specificity of 70%. The positive likelihood ratio stood at 3.1, while the negative likelihood ratio was 0.12. Hence, the model possesses diagnostic capability for both confirming and excluding a post-anaesthetic response.
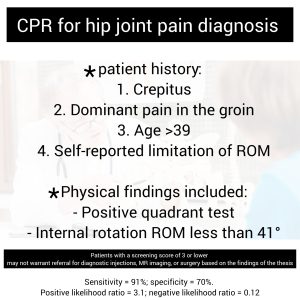
Finally, this clinical prediction rule should be treated as preliminary until it has been verified in follow-up research.
References
- Burgess, R. M., Rushton, A., Wright, C., & Daborn, C. (2011). The validity and accuracy of clinical diagnostic tests used to detect labral pathology of the hip: a systematic review. Manual Therapy, 16(4), 318-326.
- Byrd, J. W. T., & Jones, K. S. (2001). Hip arthroscopy in athletes. Clinics in Sports Medicine, 20(4), 749-762.
- Clohisy, J. C., Knaus, E. R., Hunt, D. M., Lesher, J. M., Harris-Hayes, M., & Prather, H. (2009). Clinical presentation of patients with symptomatic anterior hip impingement. Clinical Orthopaedics and Related Research, 467(3), 638-644.
- Ganz, R., Leunig, M., Leunig-Ganz, K., & Harris, W. H. (2008). The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clinical Orthopaedics and Related Research, 466(2), 264-272.
- Jaeschke, R., Guyatt, G., & Sackett, D. (1994a). User’s guides to the medical literature: III. How to use an article about a diagnostic test: B. What are the results and will they help me in caring for my patients? JAMA, 271(9), 703-707.
- Leeflang, M. M. G., Deeks, J. J., Gatsonis, C., & Bossuyt, P. M. M. (2008). Systematic reviews of diagnostic test accuracy. Annals of Internal Medicine, 149(12), 889-897.
- Martin, H. D., Shears, S. A., & Palmer, I. J. (2010b). Evaluation of the hip. Sports Medicine and Arthroscopy Review, 18(2), 63-75.
- McCarthy, J. C., & Busconi, B. (1995). The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics, 18(8), 753-756.
- McCarthy, J. C., Noble, P. C., Schuck, M. R., Wright, J., & Lee, J. (2001). The watershed labral lesion. Its relationship to early arthritis of the hip. Journal of Arthroplasty, 16(8 SUPPL.1), 81-87.
- Rahman, L. A., Adie, S., Naylor, J. M., Mittal, R., So, S., & Harris, I. A. (2013). A systematic review of the diagnostic performance of orthopedic physical examination tests of the hip. BMC Musculoskeletal Disorders, 14.
- Reiman, M. P., Goode, A. P., Hegedus, E. J., Cook, C. E., & Wright, A. A. (2013). Diagnostic accuracy of clinical tests of the hip: a systematic review with metaanalysis. British Journal of Sports Medicine, 47(14), 893-902.
- Takla A, O’Donnell J, Voight M, et al. The 2019 International Society of Hip Preservation (ISHA) physiotherapy agreement on assessment and treatment of femoroacetabular impingement syndrome (FAIS): an international consensus statement. J Hip Preserv Surg. 2020;7:631-642.
- Tibor, L. M., & Sekiya, J. K. (2008). Differential diagnosis of pain around the hip joint. Arthroscopy, 24(12), 1407-1421.
- Tijssen, M., van Cingel, R., Willemsen, L., & de Visser, E. (2012). Diagnostics of femoroacetabular impingement and labral pathology of the hip: a systematic review of the accuracy and validity of physical tests. Arthroscopy, 28(6), 860-871.
- White, S. G. (2016). The Diagnostic Accuracy of the Clinical Examination of the Hip. Doctoral dissertation, AUT University, School of Clinical Sciences. Supervisors: Professor Peter McNair, Dr. Mark Laslett.
