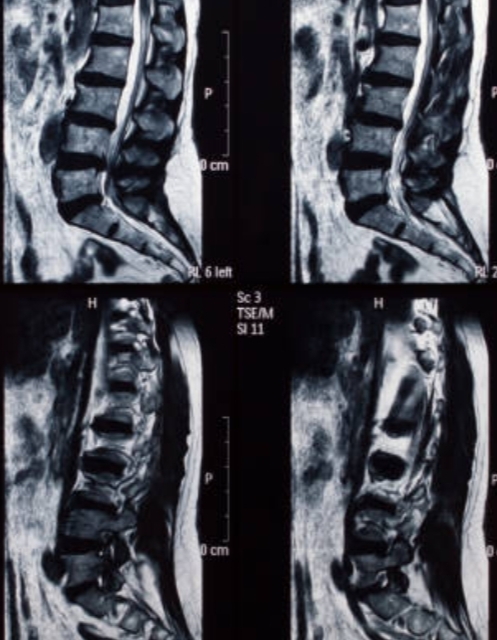
Disc displacements, often linked to back pain, can manifest as diffuse bulges or more localized herniations. Herniations are categorized into protrusions, which remain within the outer annular fibers, and extrusions, which break through the annulus fibrosus. Typically, extrusions are larger than protrusions (Fries et al., 1982).
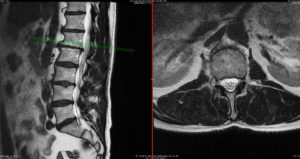
A study by Jensen et al. (1994) involving 98 asymptomatic volunteers and 27 back pain patients found that disc bulges appeared in 52% of volunteers and 76% of patients, while disc protrusions were observed in 27% of volunteers and 54% of patients. However, these differences were not significant enough to be diagnostically useful. Notably, disc extrusions were present in only 1% of volunteers but in 26% of patients, suggesting that extrusions are a more reliable indicator of symptomatic disc lesions. Porchet et al. (2002) analyzed 394 patients with sciatica and/or back pain, finding a correlation between the severity of leg pain and disability with the severity of disc abnormalities. Conversely, studies by Karppinen et al. (2001) and Modic et al. (2005) found no clear relationship between the extent of disc abnormalities and the intensity of symptoms or disability. The conflicting findings imply that the impact of a disc herniation on symptoms depends not only on the size of the herniation but also on the spinal canal’s dimensions. For instance, at levels L4-5 and L5-S1, where most herniations occur, the spinal canal’s triangular shape offers more room centrally, making lateral recess herniations more likely to cause nerve root compression. Thelander et al. (1994) and Carlisle et al. (2005) emphasized the importance of measuring the relative size of the herniation to the spinal canal’s dimensions. Their findings indicate that larger herniations tend to necessitate surgical intervention, especially in central locations.
Key Takeaways
There is no single feature that can definitively distinguish a symptomatic disc herniation from an incidental finding. However, several guidelines can help minimize misinterpretation:
- Anatomic and Clinical Correlation: Match the lesion’s location with the clinical signs, such as pain distribution, sensory loss, and reflexes.
- Size and Location: Larger extrusions are more likely to cause symptoms, but their effect also depends on the spinal canal’s roominess.
- Nerve Root Compression: Evidence of nerve root compression is crucial and may be influenced by the patient’s posture during imaging.
These insights underline the complexity of diagnosing and treating disc herniations and highlight the need for a comprehensive approach that considers both anatomical and clinical factors.
References
- Aejmelaeus R, Hiltunen H, Harkonen M et al (1984) Myelographic versus clinical diagnostics in lumbar disc disease. Arch Orthop Trauma Surg 103(1):18.
- Beattie PF, Meyers SP, Stratford P et al (2000) Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine 25(7):819.
- Carlisle E, Luna M, Tsou PM et al (2005) Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J 5(6):608.
- Fries JW, Abodeely DA, Vijungco JG et al (1982) Computed tomography of herniated and extruded nucleus pulposus. J Comput Assist Tomogr 6(5):874.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N et al (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331(2):69.
- Karppinen J, Malmivaara A, Tervonen O et al (2001) Severity of symptoms and signs in relation to magnetic resonance imaging fi ndings among sciatic patients. Spine 26(7):E149.
- Modic MT, Obuchowski NA, Ross JS et al (2005) Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 237(2):597.
- Porchet F, Wietlisbach V, Burnand B et al (2002) Relationship between severity of lumbar disc disease and disability scores in sciatica patients. Neurosurgery 50(6):1253.
- Thelander U, Fagerlund M, Friberg S et al (1994) Describing the size of lumbar disc herniations using computed tomography. A comparison of different size index calculations and their relation to sciatica. Spine 19(17):1979.