In this blog, I will discuss anatomical concerns for the peripheral nervous system, followed by a few words about the central nervous system. However, the primary focus will be on the peripheral nervous system.
A) Anatomical aspects:
Peripheral Neurons:
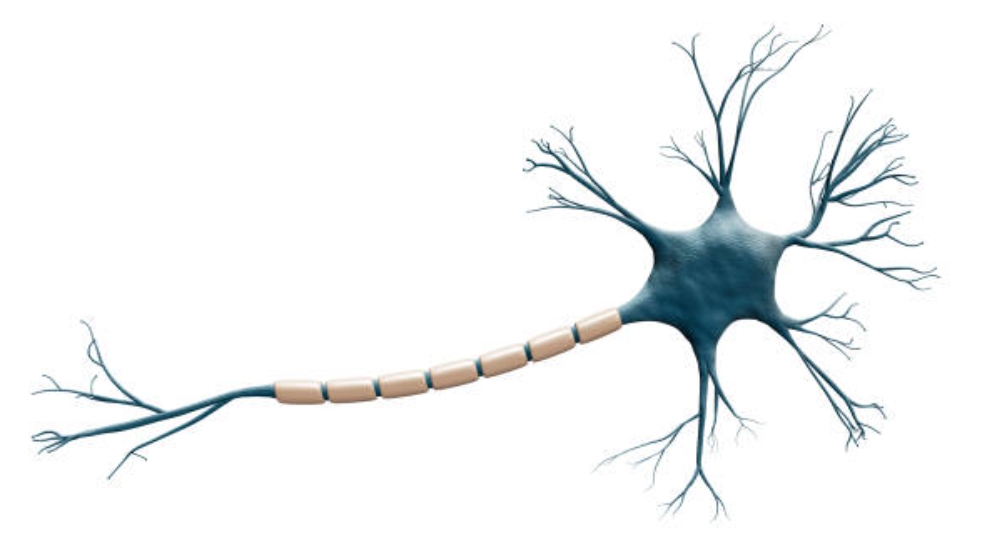
The key functional components of peripheral neurons are the axon and dendrites, as well as the cell body (in the dorsal root ganglia for sensory neurons). Another component of neurons are Schwann cells, which can be myelinating or non-myelinating. Neurons are categorised into three broad classes based on morphological and functional parameters:
Thick myelinated fibres that transmit signals to and from muscles (e.g., A fibre) and conduct sensations like touch and proprioception (Merskey H. and Bogduk N. 1994).
A fibres are sparsely myelinated fibres that convey nociceptive signals elicited by stimuli such as cold and pin prick (Hall TM and Elvey RL, 1999). Unmyelinated nerve fibres (C fibres) with small diameters that serve nociception elicited by heat or mechanical stimuli, as well as harmless temperature changes (e.g., warm detection) and itch (Attal N. et al. 2011).
C fibres aren’t just for pain. Indeed, it has recently been proposed that C fibres may mediate pleasurable touch sensations generated by skin brushing (Loken LS et al. 2009). Furthermore, postganglionic sympathetic neurons are unmyelinated axons with modest diameters that belong to the C fibre group.
Nociceptors are classified not only by their fibre diameter and myelination but also by their sensitivity to the type of stimulus (e.g., mechanosensitive, heat-sensitive, or chemosensitive) and response characteristics (e.g., low or high threshold) based on the type of ion channels present in their free nerve endings. Smith ES and Lewin GR (2009) classify C-nociceptors into four primary groups:
- C-polymodal fibres that are activated by mechanical, thermal, and chemical stimuli (Merskey H. and Bogduk N. 1994).
- C-fibres that are activated by certain modalities (e.g., mechanonociceptors, heat nociceptors, etc.) (Hall TM and Elvey RL, 1999).
- low-threshold C fibres that mediate pleasant touch (Attal N. et al. 2011).
- Silent (sleeping) nociceptors (Younes M, et al. 2006) that become sensitised to inflammatory stimuli.
Clinicians should be aware that a standard bedside neurological examination (reflex, muscle, and light touch testing) is limited to the function of large-diameter motor and sensory neurons and does not provide information on the functional or structural integrity of small myelinated or unmyelinated neurons, which constitute the majority of neurons within a peripheral nerve.
Schwann Cells and Myelin:
While both myelinated and unmyelinated axons are connected with Schwann cells, only Schwann cells in myelinated fibres create an insulating covering of lipids and proteins known as myelin sheaths. Schwann cells and axons communicate closely in areas called paranodes, which are located near the Ranvier nodes. Ranvier nodes are the spaces between myelin sheaths.
These nodes have a high density of voltage-gated sodium channels, whereas potassium channels are found beneath the myelin in the juxtaparanodes (the region next to the paranodes) (Rasband MN and Trimmer JS. 2001). Together with the myelin sheath (the internodes), this specific ion channel architecture allows saltatory action potential conduction in myelinated axons, which explains the higher conduction velocities of A and A fibres (thickly myelinated, 70–120 m/s), followed by A fibres (thinly myelinated, 6–25 m/s), and C fibres (unmyelinated, 1 m/s) (Julius D. and Basbaum AI. 2001). The unique myelination and resulting difference in conduction velocity of the two nociceptor fibre types is proposed to account for the quick, acute, and sharp pain evoked by noxious stimuli (A fibres) vs. delayed, diffuse, and dull pain produced by noxious stimuli (C fibres) (Basbaum AI and Jessell TM, 2000).
Central Nervous System:
The peripheral nervous system is closely linked to the central nervous system. Despite the fact that these two systems are anatomically distinct, they constitute a functional entity that cannot be separated.
B) Physiological aspects:
Neural Blood Circulation and Blood–Nerve Interface:
For metabolic functions like protein synthesis (e.g., neurotransmitters), neurons are largely dependent on an appropriate energy supply. While neuronal cell bodies have the highest metabolic demand, peripheral nerve trunks consume energy for active processes such as axonal transport and ion pumps to restore membrane potentials after action potential production. The nervous system has a complicated blood circulation system, the vasa nervorum, to fulfil the essential energy supply.
Radicular vessels branch off blood vessels that frequently run parallel with the major peripheral nerves to deliver blood to the peripheral nervous system. The intrinsic neural blood circulation is made up of longitudinally oriented epineural vessels that descend into the perineurium and eventually pierce into the endoneurium, which contains a dense capillary network. This network is distinguished by numerous anastomoses that ensure continuous blood flow. Capillary density and blood flow in dorsal root ganglia are higher than in peripheral nerve trunks, reflecting the increased metabolic demand (McManis PG et al. 1997).
The endoneurial compartment, unlike the epineurium, lacks a lymphatic system (Sunderland S. 1978). Because tight junctions of endoneurial blood vessel epithelium and layers of perineurial cells not only restrict but also regulate molecule exchange between the endoneurial space and blood vessels, it has been suggested that the term blood-nerve interface rather than blood-nerve barrier is appropriate (Weerasuriya A., Mizisin AP. 2011).
In contrast to the generally impermeable blood-nerve interface in distal nerve trunks, the endoneurial arteries of nerve roots, dorsal root ganglia, and sympathetic and cranial ganglia have a fenestrated endothelium, allowing a comparatively free flow of molecules (Arvidson B. 1979). Furthermore, at the subarachnoidal angle, the perineurium is thinner, and the intercellular connections of the nerve root sheaths are not as dense as those of the perineurium in the peripheral nerve trunk (McCabe JS, Low FN. 1969). As a result, these structures are vulnerable to potentially damaging plasma extravasates.
Axonal Transport:
It facilitates the transfer of payloads such as proteins produced in neuronal cell bodies but required in axons and synaptic terminals. This transport system is separated into two parts: anterograde and retrograde transport.
- Anterograde transport:
ensures the delivery of structural components and new organelles, such as synaptic boutons or ion channels, to neurons’ proximal and distal areas (Sunderland S. 1965).
- Retrograde transport:
Transports organelles and ligands from synapses or peripheral nerve ends to the cell body of the neuron (Sunderland S. 1965).
The Immune Cells of the Nervous System:
The immune system defends an organism against foreign proteins such as pathogenic microorganisms, but it also plays a vital role in the clearance of the body’s own tissue detritus (Abbas AK et al. 2007).
The blood-nerve interface regulates immune cell trafficking into the neurological system. The peripheral nerve system and its connective tissues include a limited number of resident immune cells. Mast cells, macrophages, dendritic cells, and lymphocytes are among the cells that perform a surveillance function within the peripheral nerve.
The complement system, which consists of approximately 30 different plasma proteins, is also an important component of the immune system that, when activated, causes pathogen destruction and aids inflammation (Janeway C. 2008). Some cells in the dorsal root ganglia, such as Schwann cells and satellite glial cells, can have immunologically modulatory properties.
Perivascular cells and glial cells (astrocytes and microglia) of the central nervous system are immune-competent.
References:
- Abbas AK, Lichtman AH, Pillai S. Cellular and Molecular Immunology. 6th ed. Philadelphia: Saunders Elsevier; 2007.
- Arvidson B. A study of the perineurial diffusion barrier of a peripheral ganglion. Acta Neuropathol 1979;46(1–2):139–44.
- Attal N, Lanteri-Minet M, Laurent B, et al. The specific disease burden of neuropathic pain: results of a French nationwide survey. Pain 2011;152(12):2836–43.
- Basbaum AI, Jessell TM. Part V. Pain. In: Kandel ER, Schwartz JH, Jessell TM, editors. Principles of Neuroscience. New York: McGraw-Hill; 2000. p. 472–91.
- Hall TM, Elvey RL. Nerve trunk pain: physical diagnosis and treatment. Man Ther 1999;4(2):63–73.
- Janeway C. Janeway’s Immunobiology. In: Murphy K, Travers P, Walport M, editors. 7th ed. New York: Garland Science, Taylor & Francis Group; 2008.
- Julius D, Basbaum AI. Molecular mechanisms of nociception. Nature 2001;413(6852):203–10.
- Loken LS, Wessberg J, Morrison I, et al. Coding of pleasant touch by unmyelinated afferents in humans. Nat Neurosci 2009;12(5): 547–8.
- McCabe JS, Low FN. The subarachnoid angle: an area of transition in peripheral nerve. Anat Rec 1969;164(1):15–33.
- McManis PG, Schmelzer JD, Zollman PJ, et al. Blood flow and autoregulation in somatic and autonomic ganglia. Comparison with sciatic nerve. Brain 1997;120(Pt 3):445–9.
- Merskey H, Bogduk N, editors. Part III: Pain Terms, A Current List with Definitions and Notes on Usage. Classification of Chronic Pain. 2nd ed. IASP Task Force on Taxonomy. Seattle: IASP Press; 1994. p. 209–14.
- Rasband MN, Trimmer JS. Developmental clustering of ion channels at and near the node of Ranvier. Dev Biol 2001;236(1): 5–16.
- Smith ES, Lewin GR. Nociceptors: a phylogenetic view. J Comp Physiol A Neuroethol Sens Neural Behav Physiol 2009;195(12): 1089–106.
- Sunderland S. The connective tissues of peripheral nerves. Brain 1965;88(4):841–54.
- Sunderland S. Nerves and Nerve Injury. Edinburgh: Churchill Livingstone; 1978.
- Weerasuriya A, Mizisin AP. The blood-nerve barrier: structure and functional significance. Methods Mol Biol 2011;686:149–73.
- Younes M, Bejia I, Aguir Z, et al. Prevalence and risk factors of disk-related sciatica in an urban population in Tunisia. Joint Bone Spine 2006;73(5):538–42.